25 November 2024
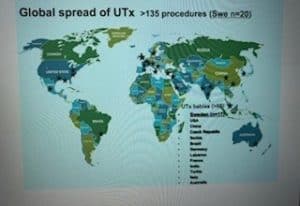
On 20 November 2024, Louisa Ghevaert attended a Progress Educational Trust event “10 Years of Womb Transplants: What Have We learned? What Does the Future Hold?”. This fascinating event looked at the important and pioneering uterine transplant work that has been undertaken over the last 10 years, starting with the world’s first successful human womb transplant and live birth in September 2014. Since then, there have been more than 135 uterus transplants around the world, including news of the UK’s first womb transplant in 2023. In doing so, uterus transplants offer hope and greater reproductive choice for women whilst raising complex medical, legal and ethical issues.
Image: Sarah Norcross, Director of Progress Educational Trust
Professor Mats Brännström provided an overview of the pioneering work done to bring the concept of womb transplant to reality. He explained that this journey started in 1998 at the Royal Adelaide Hospital in Australia, where the suggestion of a womb transplant first came up in discussions with a female patient called Angela whose womb had been removed due to cancer. This then rapidly led on to a research project looking into womb transplantation in 1999 to combat the 1 in 500 women with absolute uterine infertility factor.
Professor Mats Brännström explained that between 1999 and 2012 uterine transplant research was conducted in animals moving through mice, rats, pigs, sheep and baboons, before starting a first clinical trial in humans in Sweden in 2012. He went on to explain that whilst the first human uterus transplant actually took place in Jeddah in Saudi Arabia in 2000, it was not until 2014 that we saw the world’s first successful human uterus transplant and live birth. He explained that this involved complex vascular and surgical removal of the donor’s uterus lasting 8 – 11 hours and open surgery for the recipient lasting 3 – 5 hours. He went on to explain that following the first successful live birth in September 2014, the child in question is now a healthy 10-year old. Moreover, a total of 17 children have so far been born to date in Sweden as a result of a uterus transplant, with a surgical success rate of over 90 percent. This makes it a very effective but complex fertility treatment.
Professor Mats Brännström, Pioneer of uterus transplantation, and leader of the team responsible for the first live birth following the procedure, Professor of Obstetrics and Gynaecology at Sahlgrenska Academy at the University of Gothenburg, and Senior Consultant in Gynaecology and Reproductive Medicine at Sahlgrenska University Hospital
Professor J Richard Smith then co-delivered a session with Miss Isabel Quiroga discussing the pioneering uterine transplant work and first uterus transplant in the UK in 2023. He explained this was a 25-year journey for him and a 10-year journey for his colleague Miss Isabel Quiroga. He went on to explain that key aspects of this research work were “collaboration” and “compassion”. Their work was driven by the team’s wish to relieve the suffering of women with absolute uterine infertility factor. In doing so, it required a mix of cancer and transplant surgical skills. He explained that there are 50,000 women in the UK with absolute uterine factor infertility. Of these around 100 – 200 women per year undergo surgery, with other options being adoption or a uterus transplant. He added that women who qualified to join the UK womb transplant programme were aged 24 – 42 years old and in good health. They needed to demonstrate absolute uterine factor infertility and they must have already created embryos comprising their own eggs.
Image: Professor J Richard Smith, Joint leader of the surgical team responsible for the first uterus transplant in the UK, and joint leader of the UK Research Team at Womb Transplant UK
Miss Isabel Quiroga explained that the first successful kidney transplant took place in 1954 and it was not until 2014 (60 years later) that the first successful uterus transplant and live birth took place. She explained that it takes time to develop the relevant procedures and techniques. To date, there have only been around 135 uterus transplant cases globally over the last ten years and so it is still early on in this journey. She went on to explain that uterus transplant work in the UK took 8 years from 2014 – 2022 to secure the relevant multiple approvals required. She added that a uterus transplant is a life-creating procedure for patients who are not sick and so the risks of surgery and immunosuppression need to be managed carefully.
Miss Isabel Quiroga explained that the first UK patient recipient of a uterus transplant suffered with MRKH (meaning she was born without a womb). The uterus donor was her elder sister, who had already completed her family. The operation was carried out on a Sunday so as not to prejudice other patients and involved a medical team of 30 people on a pro bono basis. She explained that it was challenging surgery funded by Womb Transplant UK. the Oxford transplantation team handled the recipient transplant whilst the medical team at Imperial Hospital in London undertook the donor hysterectomy. Both patients recovered well and the UK now has what they hope is a sustainable programme, with hundreds of women having contacted them since to become donors.
Image: Miss Isabel Quiroga, Joint leader of the surgical team responsible for the first uterus transplant in the UK, and joint leader of the UK Research Team at Womb Transplant UK
Following this, Eleanor Findlater gave an insightful personal patient perspective about the impact of absolute uterine infertility. She explained that 20 years ago, she had to undergo a hysterectomy aged 32 years old having recently married her husband and received a diagnosis of cancer of the uterus. She spoke powerfully about the shock, devastation and fear of being childless just six months after her honeymoon and how this eclipsed everything else in life. She went on to say that she had discussions with medics who told her they were working towards the first womb transplant and how she would have had one had it been available back then. However, instead she had to look at other options of adoption or surrogacy. She added that she ruled out adoption as she learned that she would have had to wait until she was 5 years in remission from cancer. As a result, she investigated surrogacy through UK not-for-profit surrogacy agency COTS and within 3 weeks she was matched with a surrogate. Thereafter, she underwent IVF as her ovaries had been left intact and she was able to create embryos with her husband’s sperm, which were then transferred to their surrogate who gave birth to her 2 sons. She ended her session highlighting the lasting pain of being denied the fundamental experience of giving birth and how she would have had a womb transplant 20 years ago had it been a viable option, adding that it is very exciting to witness how many young women’s lives could change with the opportunity of a womb transplant.
Image: Eleanor Findlater, Patient who underwent a hysterectomy, after being diagnosed with adenosarcoma of the uterus
Dr Natasha Hammond-Browning then delivered a session looking at the legal and ethical issues associated with womb transplants. She explained that what became apparent to her was that the issues raised 10 years ago after the world’s first successful womb transplant and live birth are still the same as those being debated today. She then highlighted five ethico-legal considerations: regulation and oversight, access and funding, reproductive autonomy, donation framework and the consent process.
In terms of regulation and oversight of womb transplants, Dr Natasha Hammond-Browning explained that this raises complex issues about who should regulate these and how oversight should be carried out. It also raises questions about the right to gestate, data management and the role and benefits of a registry for uterus transplants. She went on to explain that access and funding raises further challenges about selection criteria, allocation of funding and the treatment of transgender women. She explained that uterus transplants are expensive and this raises questions about equity of access, the role of insurance and state funding. Furthermore, she explained that reproductive autonomy raises questions about whether there should be a right to gestate and if so by whom, as well as pro-natalist values which could vary from country to country. She went on to explain that the donation framework raised issues between a living donor and a deceased donor, risks for living donors, consent and opt-out systems. For example, the UK womb transplant team requires the recipient woman to use her own eggs whereas women more widely can legally use donor eggs. Lastly, she explained that the issue of consent is important. It raises a question about whether the family of a deceased should be able to consent to donation of a uterus, adding that a uterus is currently opted out of the presumed consent to donation framework in the UK.
Image: Dr Natasha Hammond-Browning, Senior Lecturer in Law, and Study Abroad Director for Law, at Cardiff University
Overall, this excellent event by Progress Educational Trust provided an enlightening and in-depth look at the evolving field of uterus transplants around the world, the majority of which are currently being carried out in Europe, the US and now the UK.
Need a fertility or modern family lawyer?
Given rapid advances in reproductive medicine and ongoing infertility and declining global fertility rates, it is more important than ever to maximise reproductive choice and make informed decisions about pathways to parenthood.
Specialist fertility and family law strategies help inform effective approaches to (in)fertility and maximise reproductive health outcomes, as well as proactively manage family building arrangements. They identify and address a range of legal and practical issues and challenges associated with family creation and fertility treatment, putting family building and life on a firm foundation and maximising successful results. In doing so, this addresses:
- Legal issues and family building options due to impaired fertility including cancer diagnosis, unsuccessful conception, age-related fertility decline, change in gender, delayed parenthood.
- Complex personal and family situations.
- Unexpected death of a loved-one and issues associated with posthumous storage and use of eggs, sperm and embryos in fertility treatment (e.g. due to an accident or illness).
- Legal issues and options associated with assisted conception involving a known donor, co-parent or identity-release or non-identifiable donor (e.g. legal parentage, parental rights, financial responsibility and dispute mitigation).
- Legal and wider aspects of international surrogacy or a UK surrogacy arrangement.
- Difficulties with storage and use of frozen eggs, sperm and embryos in fertility treatment in the UK (e.g. problems with consent).
- Issues with import of frozen gametes and embryos into the UK for use in fertility treatment and surrogacy (e.g. due to anonymous and commercially obtained gametes and embryos engaging UK public policy restrictions).
- Issues with the export of frozen gametes and embryos abroad for use in fertility treatment and surrogacy (e.g. consent and storage term difficulties).
- Legal and biological parentage issues and disputes (e.g. concerning DNA testing, direct-to-consumer genetic testing, rectification of birth certificate, declaration of parentage, step-parent adoption, recognition of overseas adoption, parental order).
- Care and upbringing of children following a dispute with an ex-partner, parent, donor or surrogate (e.g. contact, residence, financial arrangements, parental responsibility, specific issue or prohibited steps).
- Expert witness fertility, surrogacy and donor conception law services.
If you need advisory, consultancy or legal assistance to put in place effective strategies to manage preconception, fertility treatment and global family building, pregnancy, birth and family life contact Louisa Ghevaert by email louisa@louisaghevaertassociates.co.uk or telephone +44 (0)20 7965 8399.
Images: Louisa Ghevaert, CEO & Founder Louisa Ghevaert Associates