22 March 2024
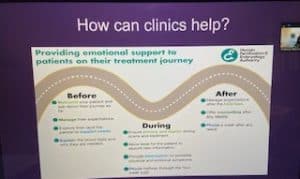
On 13 March 2023, Louisa Ghevaert was pleased to attend Progress Educational Trust’s event “Welfare of the Fertility Patient: Spotting Signs and Treatment after Trauma”. This raised awareness of the importance of considering the welfare of fertility patients and not just the welfare of the child. At present, there is nothing in the Human Fertilisation and Embryology Act 1990 (as amended) which explicitly states that the welfare of patients should be considered. Whilst counselling and standard procedures at fertility clinics can help patients navigate the normal ups and downs of treatment, there needs to be greater focus on spotting and effectively supporting signs of trauma and safeguarding patients during their treatment journeys.
Image: Sarah Norcross, Director at Progress Educational Trust
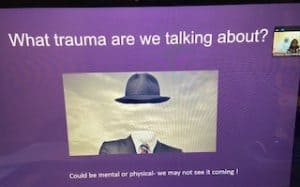
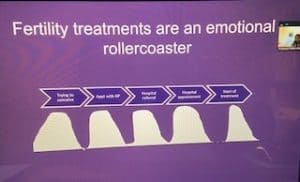
Professor Abha Maheshwari explained that trauma can often be invisible, be it emotional or physical, meaning it can be difficult to see it coming in patients. Things can be going on in the background of patients’ lives during fertility treatment that can suddenly manifest themselves, seemingly without warning. For example, she cited a case where a patient attended for an early pregnancy scan and was then shocked to learn that the patient had committed suicide because there had been no obvious indicators of trauma. She explained that there are different forms of abuse and trauma which need to be taken into account including: physical, sexual, psychological or emotional, financial, neglect and omission, discrimination and situations where people fabricate illness. Added to this, fertility treatment is already an emotional rollercoaster for people trying to conceive. It involves appointments with their GP, a hospital referral, hospital appointments and then treatment at the fertility clinic. Moreover, not all treatment works and the longer the gap between each step the more stress and anxiety can build up which makes things worse.
Professor Abha Maheshwari went on to explain that fertility patients are also bombarded with a lot of information during treatment. At the start of the process, their levels of positivity are high. However, the two week wait before finding out whether a pregnancy has been established is a long time for patients. As such, the HFEA recommends that fertility clinics call patients one week into the two week wait to check on them and provide support. If treatment is unsuccessful, it is then helpful to put a plan in place as quickly as possible to deal with patients’ anxiety. It is also important to carefully navigate situations where one patient out of a couple reveals something which they wish to keep secret from their partner or which triggers a change of heart about proceeding with treatment and ensure that specialist legal advice is obtained in these situations. Fertility clinics also need to ensure staff receive training about abuse and trauma in fertility patients and that appropriate procedures, responsibilities and reporting functions are implemented. Moreover, stress can be encountered as a couple where there is background of medical conditions.
Image: Professor Abha Maheshwari, Lead Clinician at Fertility Scotland, Clinical Director and Lead Consultant for Reproductive Medicine and Surgery at the Aberdeen Fertility Centre
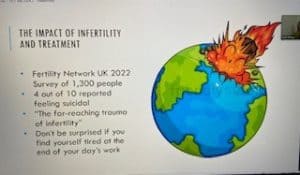
Ruth Philips, fertility counsellor at Edinburgh Fertility Centre, then gave an insightful presentation about fertility patient trauma and distress.She explained that a Fertility Network UK 2022 patient survey of 1,300 people revealed that four out of ten reported feeling suicidal during fertility treatment, demonstrating the “far reaching trauma of infertility”. Often, fertility clinics are delivering difficult news to patients and witnessing their emotional and distressed responses.
Ruth explained that signs of trauma can come to light in different ways. This can be previously disclosed sexual violence or abuse. It can also arise as a first time disclosure during fertility treatment. If so, trauma informed counselling can then be implemented. If trauma is disclosed for the first time, this has to be handled very carefully and at the patient’s own pace so they feel in control (having not been in control before). It is important to believe the patient and appreciate that it is difficult for them to speak about it. It can be helpful to gently probe “pockets of shame” which patients can be afraid to talk about and help them uncover these feelings. Patients also need to be reminded that none of this is their fault and that all of the blame, shame and responsibility lies with the perpetrator and hopefully over time they will begin to believe this too. It is also helpful to try and obtain the patient’s consent to share this with other members of the fertility clinic team so they can be on the alert about this.
Ruth explained that undergoing fertility treatment is a sensitive time for patients. They can be dealing with “disenfranchised grief” due to other sources of trauma and distress brought on by miscarriage, ectopic pregnancy, other tensions in relationships and existential crisis and grief if treatment fails. There are also outside life events that can occur during the course of treatment as well. Signs of trauma to look out for in patients include body language and change of behaviour. Asking open ended questions and carefully reviewing patient notes can also be useful. In terms of helping patients deal with trauma, Ruth explained that continuity of care with the same doctor and nurse is beneficial. It can be helpful to patients if their feelings are validated and clinic staff show empathy for their situation and feelings. It can also be helpful to explain treatment as it unfolds to restore some sense of control for patients and be honest with them about preparing for disappointment. Added to this, sometimes just sitting with a patient in silence can provide a source of comfort and support.
Image: Ruth Philips Fertility Counsellor at Edinburgh Fertility Centre
Dr Susheel Vani, Consultant Gynaecologist and Lead Clinician at the Glasgow’s Royal Infirmary’s Assisted Conception Service explained that trauma in fertility patients is a difficult topic to address because there is not a lot of evidence of this. Stressors can present differently between male and female fertility patients. For male patients, there can be a reluctance to get a sperm test and a firm belief that a lack of pregnancy is due to problems with their female partner. Men who use body building supplements can often react with disbelief that these can sometimes switch off sperm production because they feel so fit and healthy and this can create relationship issues. Men can find it difficult to accept that lifestyle changes have made no impact on their semen quality. Obese men can also struggle to accept that their obesity can be contributing to their poor sperm quality. Men with diabetes can also find it difficult to accept that this can cause ejaculatory issues. Moreover, if no sperm is found, even after a sperm retrieval procedure, this can have a big impact on a man as he may never be a biological father of a child. For couples needing donor sperm, there can also be tensions due to societal pressures, ethnic and religious beliefs.
Dr Susheel Vani then spoke about stressors encountered by women during fertility treatment. These include age and delays by the NHS which can exacerbate concerns about advancing age. Women can encounter difficulties with BMI criteria which can restrict access to fertility treatment waiting lists, together with lack of support to deal with weight issues. Women can also experience stress as a result of the nature of fertility treatment, including vaginal scans and procedures. Other stressors for women can be associated with unexplained or poor ovarian reserve at a relatively young age and the impact of the ‘biological clock’. Added to this, women can experience stress trying to find the right life partner at the right time and dilemmas over whether to freeze their eggs whilst they try to achieve stability in life. Furthermore, women can encounter stress when they find they don’t have any usable eggs and they realise they won’t become a biological parent.
Dr Susheel Vani explained that there are also stressors which fertility patient couples experience. These include situations where one partner is not ready to embark on fertility treatment. It also includes situations where one partner works away from home as this can delay treatment, especially for offshore workers. Couples can also experience significant stress if there are delays with NHS waiting lists or they receive variable support from their GPs. Welfare of the child concerns can also arise due to past history of domestic abuse, past sexual abuse, violence, criminal convictions and issues with alcohol and drugs. He went on to explain that measures that can help include clear and honest discussions at the start of the fertility treatment journey, building a good rapport within the same medical team, access to specialist support and counselling, a multi-disciplinary approach, unbiased discussions about private treatment options and early information about any regulatory issues affecting them if mistakes happen.
Image: Dr Susheel Vani, Consultant Gynaecologist and Lead Clinician at the Glasgow’s Royal Infirmary’s Assisted Conception Service
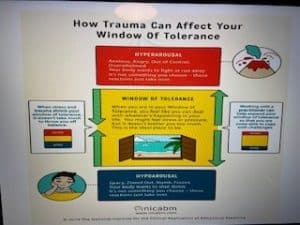
The final session was delivered by Nicole McKeith, a Fertility Nurse, and Nurse Sedationist, at Ninewells Hospital’s Assisted Conception Unit. Nicole explained that she led a trauma informed practice supporting patients with a history of sexual violence and abuse. She explained that fertility treatment can trigger past trauma, for example in undergoing egg collection under sedation it can bring back memories of alcohol and rape happening. She went on to say that trauma impacts an individual’s development and it can affect their engagement with healthcare services. Everyone has a window of tolerance enabling them to function from day to day. Outside of this window of tolerance, people can experience hyper-arousal. This is where they feel unable to cope and become erratic, overwhelmed and out of control. Alternatively, outside of their window of tolerance they can experience hypo-arousal, where they shut down and are unable to speak or make eye contact and become zombie like. Nicole explained that people affected by trauma have a smaller window of tolerance than other people. Added to this, they have no control over their window of tolerance and their body takes over.
Nicole explained that meeting patients experiencing trauma with empathy and support can help them not to suffer as much trauma related symptoms. Use of language, smells, questions posed and management of sedation can take patients back to an unhappy time. Sedation can be a big trigger for fertility patients because it takes away their control and reminds them of a time when they can’t remember what happened or have gaps and this can cause anxiety and worries. Certain tests and scans, for example speculum examination, can also create issues for patients where there has been a lack of intercourse in the past, making it important to work with patients at their pace and help them feel more empowered and in control. In addition, steps like the completion of a pre-assessment questionnaire, continuity of staff, and being first on the theatre list can also be helpful.
Image: Nicole McKeith, a Fertility Nurse, and Nurse Sedationist, at Ninewells Hospital’s Assisted Conception Unit
Need Advisory & Consultancy, a Fertility, Surrogacy or Modern Family Lawyer?
If you need advisory, consultancy or legal assistance to put in place effective strategies to manage preconception, fertility treatment and global family building, pregnancy, birth and family life contact Louisa Ghevaert by email louisa@louisaghevaertassociates.co.uk or telephone +44 (0)20 7965 8399.
Images: Louisa Ghevaert, CEO & Founder Louisa Ghevaert Associates